Case Study
Layered Insights Give Enrollment Experience a Competitive Edge
The Client & Challenge
Customer experience leaders at a nationwide health insurance company needed to present internal stakeholders with a unified account of existing CX data and insights to guide integrated enrollment growth plans.
The data and insights were housed with multiple internal and external sources, making it particularly challenging to present a clear view of CX along the entire member enrollment journey. However, it was critical that the decision makers understood the member journey from all viewpoints to aid in strategic planning, performance tracking, and ensuring products and services aligned with evolving customer needs.

The Solution
Ultimately, what our client needed was a holistic, easy-to-follow story of their entire enrollment experience. To achieve this, we set out to accomplish the following four core objectives:
- Developing a comprehensive research roadmap across the enrollment process
- Uncovering connection points between employee, consumer, employer, and broker experiences impacting enrollment
- Addressing critical CX, EX, and other stakeholder pain points
- Supporting development of a cross-functional action plan to enhance the enrollment experience
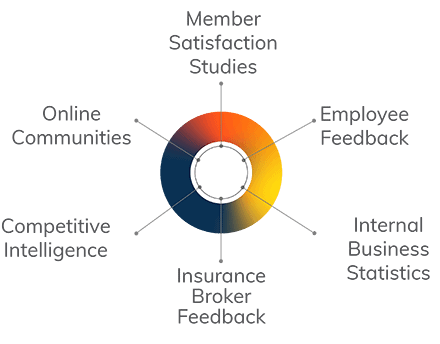
To achieve our objectives, we analyzed and integrated critical information across the health insurance company’s CX and EX research programs, competitive intelligence, and internal business data. We also synthesized a wealth of client information on the enrollment process gleaned from satisfaction tracking studies, feedback from online communities, and other proprietary research studies.
The Wins
From our analysis and data integration, we developed a cohesive, multi-faceted enrollment experience story, shared with stakeholders through socialized reporting.
Our client was able to leverage key connections we uncovered across resources to give their stakeholders a heightened, more nuanced perspective of the enrollment experience. One key insight was that the consumer’s definition of enrollment goes way beyond simply signing up for health insurance. To our client’s target markets, enrollment included researching, comparing options, and seeking answers to a wide variety of questions. Additionally, other critical insights uncovered relationships between consumer and employee pain points that called for coordinated resolution strategies.
Most importantly, the synthesis of such valuable feedback from customers, employees, and other players in the enrollment journey enabled the company to improve the overall enrollment experience in new ways and, in the process, further enhance brand perceptions.
Let's Connect.
It all starts with a conversation.
